- News 2023
- Facts & Figures
- Organisation
- Profile
- Focus 2023
- Downloads
-
Inhalte teilen:
Virtual
Medicine
Gaming and film enthusiasts have been exploring virtual worlds with VR headsets for many years. However, virtual reality can do more than just entertain; it can also save lives. At the Heidelberg University Hospital (UKHD), surgical specialists prepare for complex operations in virtual environments, and students practice medical emergencies.

Dr. Stefan Mohr uses a slider to control the physical functions of the virtual patients on the computer.
The training resembles a game of charades. Two students wearing virtual reality (VR) headsets move their arms in the air and reach into empty space. Outsiders can follow what’s happening in the world the students see through their headsets on a monitor. On the screen, one can observe the students treating burn wounds, attending to unconscious patients, or managing heart attacks or allergic shocks.
For the past two years, students have been able to complete training in the elective course “Emergency and Intensive Care Medicine” at the VR Lab of the Medical Faculty Heidelberg (MFHD). Using VR headsets and software, they learn the necessary steps to help someone in a life-threatening situation in the virtual world. If participants take the correct action, the virtual patient's body changes accordingly. Using a slider, the trainer at the control desk adjusts the patient's physical responses. A swelling decrease or the skin regains color.
“Thanks to this simulation, students can treat medical conditions in virtual training that we previously could hardly replicate,” says Dr. Matthias Huck, senior anesthesiologist and scientific director of the Heidelberg VR Lab at the Medical Faculty.

„Thanks to VR simulations, students can treat medical conditions in virtual training that we previously could hardly replicate.“
Pilot Project with Potential
So far, medical trainees primarily work with mannequins that lie on the floor in the real world. The training instructors can only describe the symptoms the dummy should exhibit, leaving participants to create a mental image and initiate the correct steps. This method cannot adequately represent every life-or-death situation.
In a few years, it might be possible to bring participants from different locations into a shared virtual space for training. The technology is already available, but public networks are not yet capable of handling the large data volumes involved, explains Jörg Miebach, the technical director of the VR Lab.
Miracle Headsets
Virtual reality (VR) headsets, also known as VR goggles, provide users with a highly realistic view into a digitally created reality. A lens in front of each eye gives the impression of being in a specific environment, while a mount ensures that the virtual space moves with every head movement, creating a 360-degree experience. VR headsets became well-known in the gaming scene. Nowadays, they are also used in science and industry.

Advantages of Mixed Reality
While emergency scenarios can be realistically portrayed in virtual reality, the tactile components are missing. Virtual bodies can be examined but not physically touched. This is possible in mixed reality (MR), a combination of virtual and real worlds.

The more realistic the training, the better prepared the medical personnel are for the mission.
A European project involving the UKHD is pursuing this approach. Participants wear VR headsets and are confronted with specific situations – such as an accident in a tunnel or on a country road with multiple casualties. The virtual view is supplemented by real mannequins that are part of the scenario.
Participants perform all tasks with their own perception, such as tilting a mannequin’s head or checking its pulse. The sensor-equipped dummies respond to these actions, for example, by restoring breathing sounds. “This technology allows us to represent a wide range of scenarios,” says Dr. Stefan Mohr, senior anesthesiologist and project supervisor.

In one exercise, for example, a triage situation was practiced – a highly stressful situation for rescue workers as they have to decide whom to help first or whom they can still help at all. “To make appropriate decisions, confidence in one's actions is needed,” says Mohr. The more realistic the training, the better the medical staff is prepared for real deployments.
Operation on a Virtual Heart
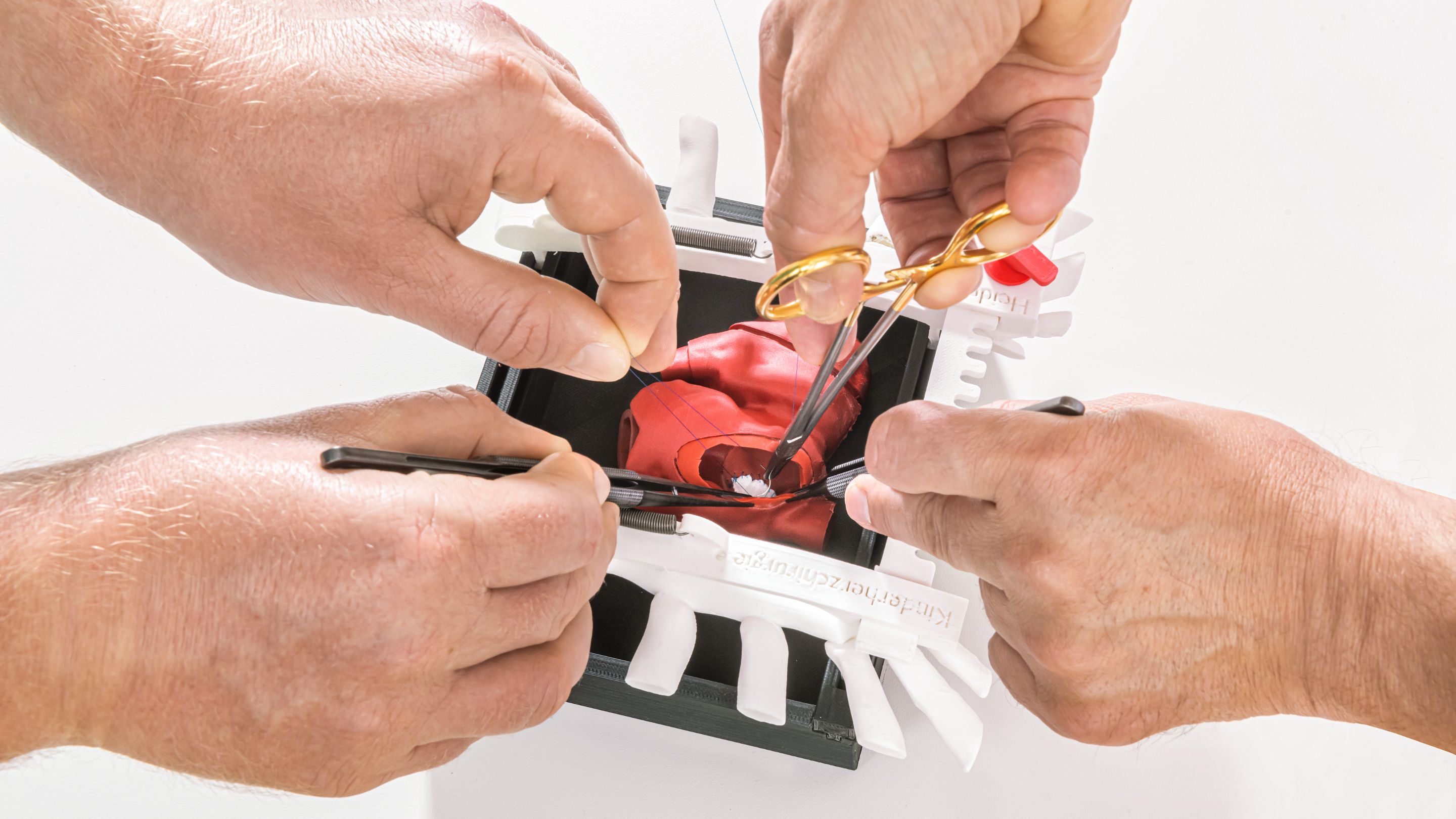
Preparing as perfectly as possible for real-life scenarios is also the goal of Professor Tsvetomir Loukanov. His team performs surgeries on newborns with complex heart defects at the UKHD. These risky operations often last between six and twelve hours. The quicker and more precise the surgery, the higher the chances of success. Therefore, Professor Loukanov and his team frequently practice their techniques on silicone models that look exactly like the affected child’s heart.
The three-dimensional models, virtually twins of the affected children’s hearts, are generated from magnetic resonance imaging (MRI), computed tomography (CT), or ultrasound data. This allows a three-dimensional image to be displayed in the virtual space, providing a much more detailed preparation. For particularly difficult operations, the surgical team can create a plastic or silicone heart model using a 3D printer.
How Common Are Heart Defects?
7900
Each year, one percent of all children in Germany are born with a heart defect – a total of 7,900 boys and girls.
Fördergemeinschaft Deutsche Kinderherzzentren e. V.
Anatomy you can touch: The heart in 3D
For particularly difficult procedures, the surgical team can have a plastic model of the heart produced by the 3D printer.
Click and drag the heart to rotate it.
Every Case is Individual
Most operations performed by the chief physician and his team are unique cases that even experienced specialists have never encountered before. “There are about 100 different congenital heart defects,” says Loukanov. These can theoretically occur in billions of different combinations.
Sometimes Professor Loukanov meets with his assistants on weekends to practice cuts and stitches on the silicone model. For complicated cases, he has several walnut-sized children’s hearts printed. If something goes wrong in the rehearsal, they repeat the procedure on a spare heart. “On the day of the operation, however, we only have one chance.”
Developed Their Own 3D Printing Method
Professor Loukanov and his senior physician Philippe Grieshaber received additional training at US clinics, where 3D models have been used to prepare for complex surgeries for years. However, the methods used in Boston or New York have a downside: they are very expensive. “The special 3D printers cost $400,000, and a single printed model currently costs $600-1,000,” says Loukanov. This is difficult to finance in the German healthcare system.
He tasked a motivated doctoral student with developing a more cost-effective method. The project was successful. The hearts can now be virtually displayed and printed three-dimensionally on a standard device for around seven euros.
Virtual practice could also shorten learning curves. “Few young doctors are interested in a career in pediatric heart surgery,” says Loukanov. One reason is the extensive training, which can last ten, sometimes fifteen years. By using 3D-printed models, future specialists could perform surgeries much faster. As a result, surgical training on patients can be more efficient and conducted with the highest possible safety. In the future, it is expected that training on simulators, already recognized in emergency medicine, will be included in the training catalogs for surgical specialties as well.
Changing Bandages on Lake Constance
Nursing at the UKHD also employs virtual reality: in the Surgical Clinic, nurses use VR headsets during bandage changes. Patients experience, for example, a virtual boat tour on Lake Constance through the 3D headsets. This helps them feel less pain and reduces the need for pain medication.
Between VR and reality
From time to time, it can be helpful to change your perspective. With the help of VR glasses, the dreary hospital room is transformed into a rippling waterscape in an instant, taking your mind off pain and worries.