- News 2023
- Facts & Figures
- Organisation
- Profile
- Focus 2023
- Downloads
-
Inhalte teilen:
Ms. Schmidt’s
Dream
of Snorkeling
People with rare diseases often carry an especially heavy burden. The Center for Rare Diseases at the University Hospital Heidelberg connects 18 specialized centers, offering hope and help to those affected. Maren Schmidt* is one of them. The 26-year-old has Loeys-Dietz syndrome, a rare genetic connective tissue disorder with a high risk of life-threatening aneurysms of the aorta. The center‘s team has saved her life multiple times. *Name was changed
4 million people in Germany suffer from one of about
8000
rare diseases.
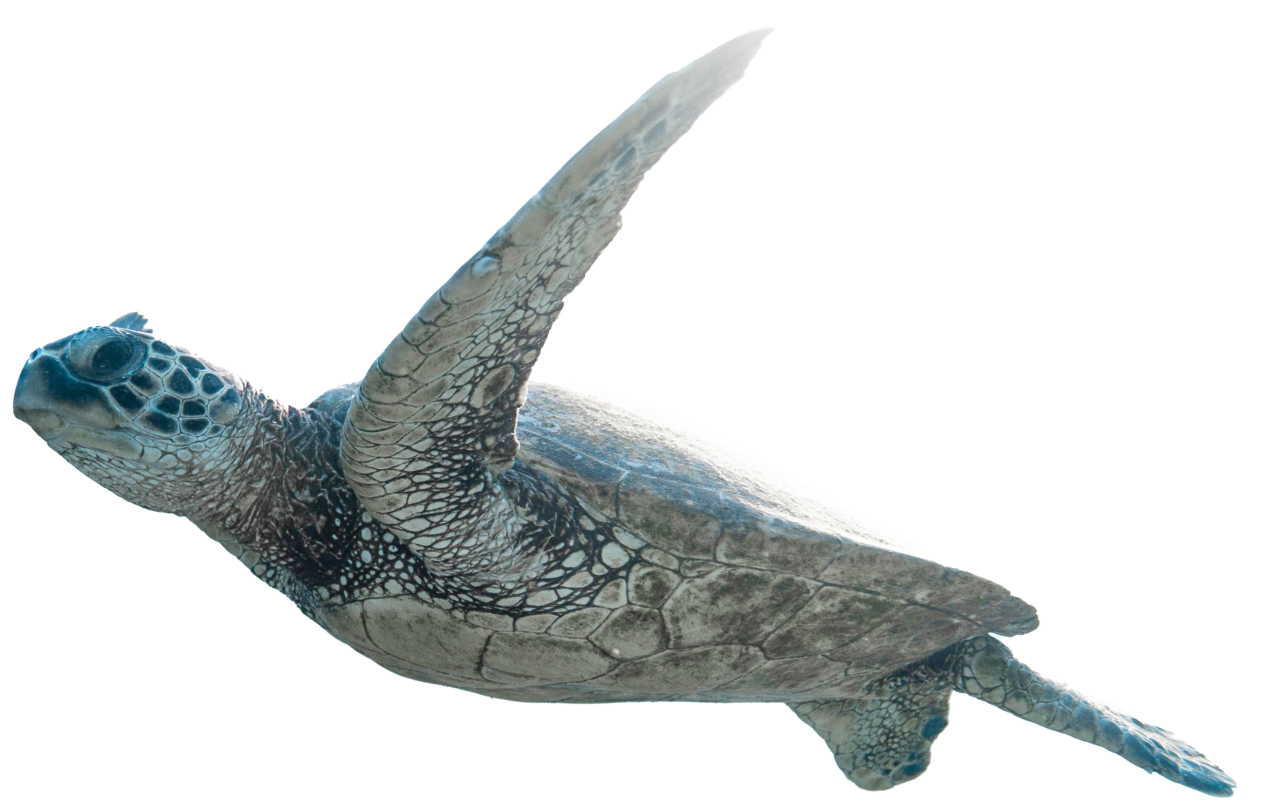
When Maren Schmidt's kidneys failed, she dreamed of rushing rivers every night. “I could only think about water,” says the 26-year-old. In her dreams, she dips her feet into cool water or swims in the sea. In reality, she had to undergo dialysis and couldn't drink much. Thirst was her constant companion. To distract herself, she watched documentaries about diving. This led to her greatest wish: to swim with sea turtles. However, she is currently unable to travel and spends many months in the hospital because of her extremely rare Loeys-Dietz syndrome.

Unclear Diagnosis in Childhood
Her medical journey began at age 13 when she was admitted to the University Hospital Heidelberg for severe abdominal pain. Initially, doctors suspected a common appendicitis. Despite the early suspicion of Klippel-Trénaunay-Weber syndrome, a rare congenital vascular disease, Maren had been healthy except for some varicose veins and swelling in her right leg. “The examinations revealed that I didn't have an inflamed appendix but an aortic aneurysm,” she recalls. An aortic aneurysm, an expansion of the aorta in the abdomen, is very unusual at her age.
Surgery was not yet necessary, but at 15, Maren had to undergo vascular surgery because her aorta, measuring over five centimeters in diameter – normal for her age is 1.5 centimeters – was at risk of rupturing, which would be life-threatening.
“We replaced the diseased segment of the artery with a synthetic graft,” says her doctor, Professor Dr. Dittmar Böckler, Medical Director of the Clinic for Vascular and Endovascular Surgery at the University Hospital Heidelberg (UKHD). “After that, I had ten years of peace,” adds Maren.

Professor Dr. Philipp Erhart

Twice, Maren Schmidt‘s condition deteriorates so dramatically that she is picked up by rescue helicopter and flown to Heidelberg.
>
10000
patients are treated annually at the Center for Rare Diseases.
Series of Surgeries
After the surgery, she returned to Heidelberg for check-ups every one to two years. During one of these visits, it became apparent that another part of the aorta needed to be replaced. In autumn 2023, she underwent successful surgery. However, once home, her health took a severe downturn: her kidneys and liver failed, and her heart weakened significantly. “I was airlifted to Heidelberg,” she recalls. She received successful treatment in cardiology (Director: Prof. Dr. Norbert Frey) and was later discharged, but now required dialysis.
A week later, she suffered an aortic dissection, a tear in the inner layer of the aorta. Her condition was life-threatening, and she was again airlifted to Heidelberg, where the cardiac surgery team (Director: Prof. Dr. Matthias Karck) performed emergency surgery. Since then, she has spent months in the hospital, undergoing planned follow-up surgeries, with complications in wound healing due to the connective tissue disorder. Fortunately, her kidneys improved, and she no longer needs dialysis.
Strongly connected
Various medical disciplines work closely together to ensure comprehensive and effective treatment. This is the only way to keep the complex symptoms of Loeys-Dietz syndrome under control. For there is currently no cure.
Interdisciplinary Collaboration
Only recently did Maren learn that she has Loeys-Dietz syndrome instead of Klippel-Trénaunay-Weber syndrome, thanks to genetic testing conducted by the Center for Rare Vascular Diseases, led by Professor Dr. Philipp Erhart, in collaboration with the Institute of Human Genetics (Director: Professor Dr. Christian Schaaf). Loeys-Dietz syndrome is a very rare genetic disorder affecting one in a million people, says Professor Erhart. At the Center for Rare Vascular Diseases, he has diagnosed this syndrome in only one other patient. It affects the connective tissue, potentially causing problems with blood vessels, the cardiovascular system, the skeleton and other organs.
Life-threatening complications include arterial tears due to the genetic defect weakening artery walls. “Ms. Schmidt also has other affected organ systems, involving cardiologists, nephrologists, gynecologists, radiologists, and heart surgeons in her treatment,” explains Professor Erhart. Regular interdisciplinary case conferences determine the next steps. Because the arteries needing treatment are very vulnerable, surgeries must be carefully planned and intensively prepared to ensure efficient and complication-free procedures.

Since Loeys-Dietz syndrome affects several organs, interdisciplinary cooperation is required not only during the operation, but also before and after.
A disease is considered rare if it affects no more than
5
in
10,000
people.
In the video, the Department of Vascular Surgery and Endovascular Surgery introduces itself together with nursing and its partners from surgery and anesthesiology at the UKHD.
Current medicine reaches its limits in treating Loeys-Dietz syndrome, regret the doctors: “Unfortunately, there is no causal therapy for this genetic defect. The disease can only be treated surgically and a best interdisciplinary complementary therapy, with lifelong follow-ups to monitor new vascular changes.” Maren will soon receive an endoprosthesis in the thoracic aorta to prevent further expansion and a potential rupture in the remaining untreated section. “This is a minimally invasive procedure,” explain vascular surgeons Böckler and Erhart.
Maren describes herself as a positive person, but the many months in the hospital have taken their toll: “It does something to you.” The numerous surgeries leave her often tired. She lacks the concentration to read a book or watch a whole movie. She spends her long hospital days doing origami, browsing Instagram, and watching documentaries. Her parents and two brothers, who visit daily, give her strength: “If it weren't for my family, I wouldn't be so optimistic.”
The Center for Rare Diseases unites the centers of expertise for …
- … Amyloidosis
- … Rare Blood Diseases
- … Echinococcosis and Rare Tropical Diseases
- … Congenital Endocrinopathies
- … Rare Heart Diseases
- … Rare Craniofacial and Orofacial Diseases
- … Rare Lung Diseases
- … Cystic Fibrosis
- … Congenital Kidney Diseases
- … Rare Orthopaedic Diseases
- … Rare Inflammatory Rheumatic Diseases
- … Chronic Hiccups
- … Congenital Metabolic Diseases
- … Syndromic Developmental Disorders
- … Rare Tumor Diseases
- … Rare Neurological Diseases
- … Rare Vascular Diseases
- … Rare Congenital Malformations of the Digestive Tract

Snorkeling with Turtles
The genetical blood test results surprised and scared Maren: “I didn't know what new restrictions might come.” She must continue to avoid putting too much pressure on her vessels. Endurance sports like swimming, hiking, and cycling are recommended for Loeys-Dietz syndrome in consultation with cardiologists, but contact sports like soccer or handball and deep diving due to underwater pressure are off-limits.
One thing delights this water fan: “Snorkeling is allowed.” Once she leaves the hospital and completes rehab, Maren dreams of snorkeling with turtles in the Mediterranean, preferably in Greece, her mother's ancestral home. She and the team at the University Hospital Heidelberg's center work daily to make this dream come true.

“A Diagnosis Is Also Important for Mental Health”




